Chances of Getting Pregnant Following Houston IVF Treatment
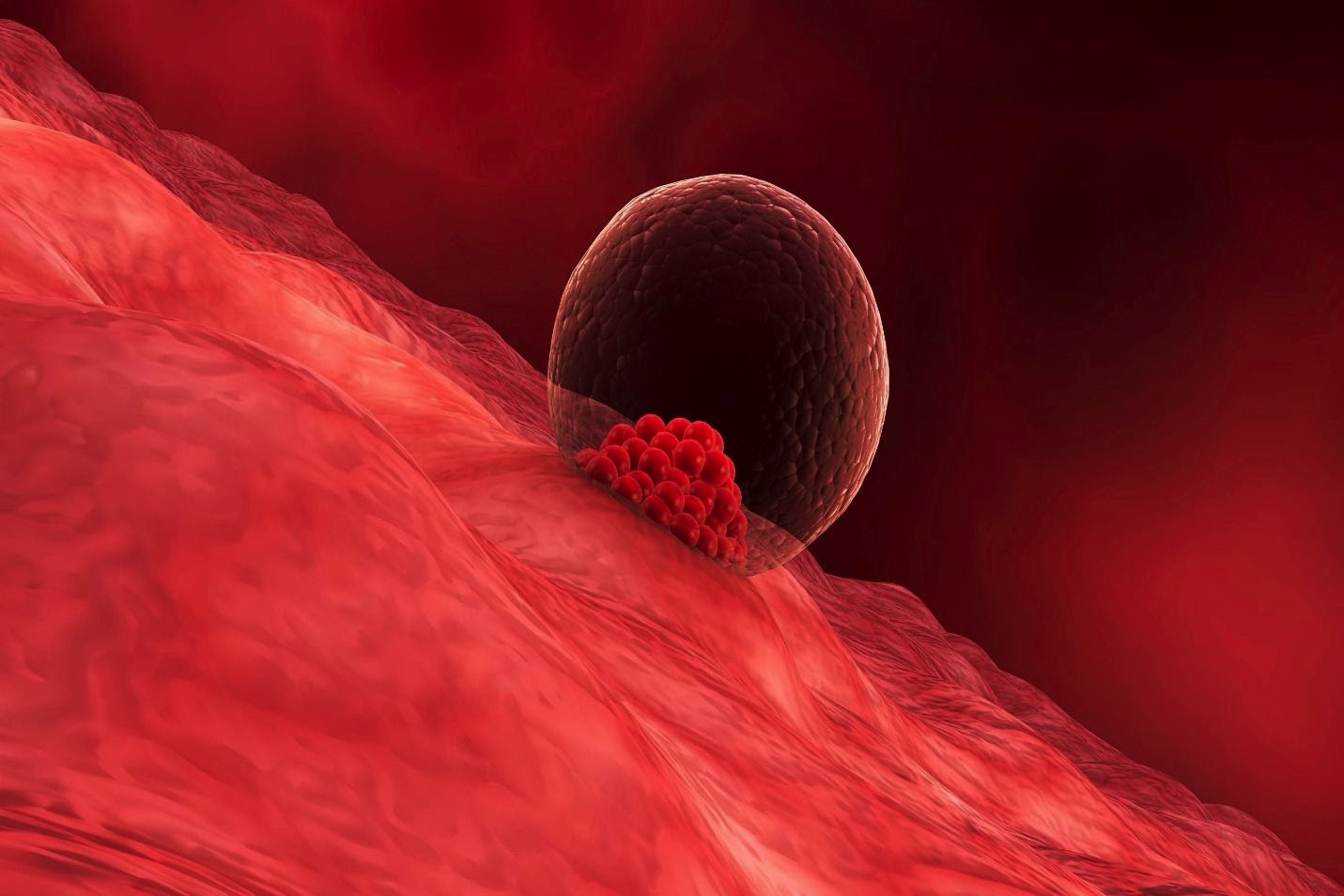
One of the most common questions patients ask following IVF treatment is “What are my chances of getting pregnant? Do I need to store more embryos?” Though there are a multitude of variables which affect the answers to these questions (age, prior history of pregnancy loss, cause of infertility, desired number of children, and more), our patients deserve an evidence-based response which may shed light on their potential to conceive. Thankfully, with decades of data collected through a variety of institutions, we are able to better answer this question.
 Few would deny that over time, advancements in the field of reproductive medicine have increased a woman’s chance of conceiving dramatically since its debut in the 1980’s. Changes in monitoring and retrieval techniques as well as fertilization procedures and embryo freezing/thawing protocols in the laboratory have played essential roles. With the advent of PGT-A (preimplantation genetic testing for aneuploidy), physicians are able to reduce the likelihood of chromosomally abnormal early pregnancies and miscarriages. Of interest are the findings from recent data accumulated and analyzed by Reproductive Medicine Associates (RMA), which revealed that women who have 3 normal embryos by PGT-A analysis have a 94.9% chance of achieving a pregnancy, regardless of age. Additionally, the same research team found that pregnancy rates were higher in patients following transfer of their first embryo than those needing subsequent embryo transfers for failed prior transfer. In short, you need at least 3 genetically normal embryos to have 1 clinical pregnancy.
Few would deny that over time, advancements in the field of reproductive medicine have increased a woman’s chance of conceiving dramatically since its debut in the 1980’s. Changes in monitoring and retrieval techniques as well as fertilization procedures and embryo freezing/thawing protocols in the laboratory have played essential roles. With the advent of PGT-A (preimplantation genetic testing for aneuploidy), physicians are able to reduce the likelihood of chromosomally abnormal early pregnancies and miscarriages. Of interest are the findings from recent data accumulated and analyzed by Reproductive Medicine Associates (RMA), which revealed that women who have 3 normal embryos by PGT-A analysis have a 94.9% chance of achieving a pregnancy, regardless of age. Additionally, the same research team found that pregnancy rates were higher in patients following transfer of their first embryo than those needing subsequent embryo transfers for failed prior transfer. In short, you need at least 3 genetically normal embryos to have 1 clinical pregnancy.
Worldwide, the average age of “first-time” mothers has been increasing. The most common reason for this shift is simple…education. Women today are postponing child-bearing for their careers. However, you’ll be relieved to know that studies performed by Cornell researchers show that the age at which eggs are retrieved has no statistically significant effect on implantation rates or clinical pregnancy rates when transferring embryos that are known to be chromosomally normal. This data may affect a patient’s decision to store more embryos for future use.
Additionally, researchers have also found that, despite PGT-A (genetic) testing to identify euploid or “normal” embryo status, not all embryos are created equal. Embryos biopsied on Day 5 or Day 6 differed from embryos permitted to grow and biopsied on Day 7. Parameters of implantation, clinical pregnancy and live birth rates were lower for those embryos biopsied on Day 7 (Flisser et. Al, Human Reproduction, 2019).
The use of frozen embryo transfers has also been gaining popularity for physicians and patients alike. Not only does it ease the scheduling process for both parties involved, but studies show that frozen embryo transfers may be associated with a slightly increased pregnancy rate given the more hormonally physiologic environment to which the embryo is exposed. Endometrial development is also thought to be more appropriately synced. Additionally, frozen embryos permit for time needed to complete genetic testing.
For some individuals, multiple IVF cycles are needed to attain 3 normal embryos. The cost of medications and procedures only add to the stress of infertility and the waning hopes of getting pregnant. Fortunately, when single cycle outcomes are compared to multi-cycle outcomes, the outcomes are the same…individuals who had transferred a genetically normal embryo obtained from one cycle or following multiple cycles are similar implantation and clinical pregnancy rates.
Between building your career, traveling, and, oh yeah, trying to find the right partner, it can be pretty difficult to prepare for the future. At HART Fertility, our goal is to help you make the best decision to support your future family goals. Whether you are actively trying to conceive or just having a “back up plan”, let us help you.




